Tackling inequalities in osteoporosis care
The problem

Postcode lottery for high quality Secondary Fracture Prevention
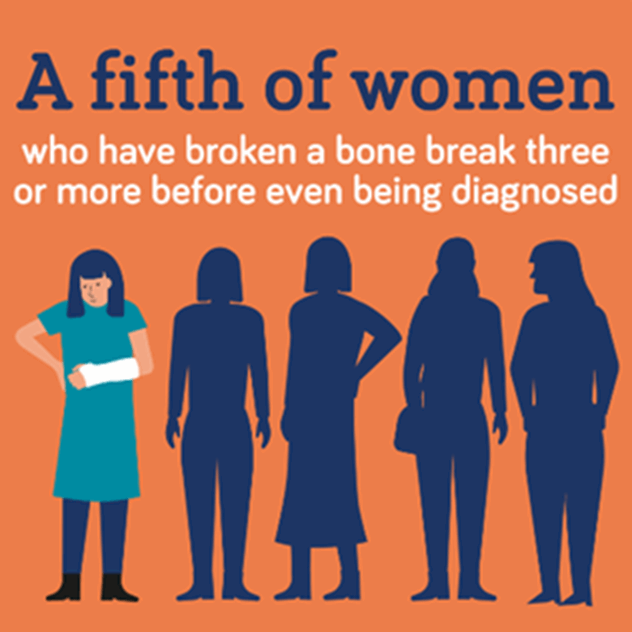
Fracture Liaison Services (FLS) are the world standard model for systematically identifying and assessing people aged 50 and older who have had a fragility fracture, and delivering a personalised treatment plan to prevent further fractures. The FLS model is a proven game-changer, reducing the risk of re-fracture by between 30-40%. However, we know that a fifth of women who have broken a bone, break three or more before even being diagnosed. This is because after the first fracture there is a postcode lottery for access to a FLS. Having access to an FLS is not the whole solution. The effectiveness of the FLS model depends on the quality of the service provided and accessibility to treatments, and like coverage, this is also a postcode lottery. There is evidence that the pandemic has worsened inequalities still further. With our ageing population, osteoporosis will put an increasing burden on the NHS – currently £4.5bn and projected to rise steeply.
Postcode lottery for high quality hip fracture care
Each year more than 70,000 older adults are admitted to a UK hospital after a hip fracture. Research has shown that how well patients recover after a hip fracture varies enormously across England and Wales. For example, in some hospitals one in ten patients died within a month of their fracture. The time patients spent in hospital and also the chance of patients needing to come back into hospital after getting home also varied widely. Patients should be able to expect to receive the same, high-quality care if they break their hip, irrespective of where they live or which hospital they attend.
People at high-risk falling through the gaps
Individuals with other medical conditions are at higher risk of falling and breaking bones. There remains a lack of clear evidence based clinical guidance for high risk groups who are particularly susceptible to osteoporosis and breaking bones.
The solution
Put the areas and people with the deepest health inequalities at the front of the queue, focusing on where there is greatest need to ensure access to osteoporosis care is equal across the UK. For example, investing in universal secondary fracture prevention coverage and achievement of these quality standards will pay for itself multiple times over: for every £1 spent on FLS, the taxpayer can expect £3.28 back.
I do wonder whether, if I had been referred for a scan six years ago, my osteoporosis might not have been given the opportunity to advance as far as it has.
Active projects
Tackling health inequities in hip fracture care delivery and patient outcomes

Principal Investigator: Dr Rita Patel, University of Bristol
Timescale: May 2024 – November 2026
Amount: £77,986
Summary: Breaking a hip after a fall is often the first sign of osteoporosis. Some groups of people spend longer in hospital, are less likely to get back home, and/or more likely to die after breaking a hip compared to other groups. Older men, people from poorer regions and some ethnic groups, have worse outcomes. These outcomes after a hip fracture are not inevitable. Using data from NHS hospitals and the national hip fracture audit we will compare how people recover after a hip fracture depending on their ethnicity, age, sex, living in a deprived area, and hospital attended. By studying how these factors influence patient services and outcomes, we will identify key factors to target to improve equitable access to high quality care for all, responsive to patient need. We will build new freely available quality improvement tools, to help hospitals critically examine potential inequalities in their services. Using our resources and checklists, and working with local stakeholders, hospitals will be able to select and implement approaches to help close identified gaps in care. This proposal directly addresses the Breaking the Silence strategy; we will tackle the postcode lottery of hip fracture care, driving-up standards and improving access to care.
Bettering Our uNderstanding of ostEoporosis (BONE) study: Use and patient experience of romosozumab in the NHS

Principal Investigator: Dr Muhammad Kassim Javaid, University of Oxford
Timescales: May 2024 – November 2027
Amount: £91,809
Summary: Osteoporosis significantly impacts the lives of patients and their families. For patients living after menopause who have severe osteoporosis and then have broken their hip, shoulder, wrist or spine, the NHS now recommends a new medicine called romosozumab. However, there are concerns that some patients who should be offered romosozumab are not because of where they live or other reasons such as their age. We want to find out how romosozumab is used in the NHS and the patients' and clinicians' experiences to see where the differences are and what is causing them. With patient and public involvement throughout, we will develop an easy-to-use, secure online website. Using the website, we will ask patients who have been offered or prescribed romosozumab to consent and answer questions about their osteoporosis, treatments and other conditions. We will also ask their medical teams to enter their laboratory tests and bone scans from medical records. We will invite some patients and clinicians to focus groups to understand their experiences and decision-making better. The results will improve how the NHS improves access to and experience of romosozumab treatment in high-risk patients, benefiting patients, their families, the NHS and wider society.
Objective physical activity measurement in a feasibility randomised controlled trial of outdoor mobility after hip fracture

Principal Investigators: Professor Katie Sheehan, Dr Rhian Milton-Cole (Queen Mary University of London) and Dr Emma Godfrey, Kings College London
Timescale: June 2024 – August 2025
Amount: £29,485
Summary: Why are we doing this study? People who broke their hip said they felt better once they could get out of the house again. Healthcare after a broken hip rarely includes support to go outside. We got funding for a study to see if it is possible for the NHS to support people who break their hip to get back to going outside. Here we ask for ‘top-up’ funding to allow better measurement of how much physical activity people do (and where) during this study. What will we do? We will invite 20 people to take part. We will send them a wrist-worn motion sensor (watch without a face) to wear for 10-days at four time points. During this time, people will be in telephone contact with the research team. We will ask them to send the sensor back by prepaid courier. We will get activity data from the sensor. We will compare data between those receiving regular and extra care. What is the next step? If this study shows we can collect this data, we will include it in a larger study to see if the extra care helps people get back to going outside and be more active.
Recently completed projects
Using real world audit data to identify the high-risk fracture patients and determinants of effective and efficient secondary fracture prevention

Principal Investigator: Dr Muhammad Kassim Javaid, University of Oxford
Timescales: June 2022 – September 2024
Amount: £70,092
Summary: Five hundred thousand adults break a bone after falling every year in the NHS. This could be first sign of osteoporosis. The NHS funds Fracture Liaison Services (FLSs) to provide osteoporosis checks for patients after a broken bone. We have shown significant differences between FLSs with only 1:10 patients receiving the highest standards of care. This research has two aims to improve how well FLSs work. Firstly, we will explore the factors that predict FLSs providing good care. We will use national FLS surveys that measure patient care after they have broken a bone. We will compare the structure of FLSs with how well they manage patients. We will review the results with FLS staff and patients explore other potential factors that could influence how well an FLS works. Secondly, we will try to find a group of patients at very high risk of breaking another bone. These patients may need faster and stronger treatments. To do this, we will look at patients treated by the FLS but still break their hip in the next two years and describe what was different about them. The results will help FLSs update their patient pathways to better manage this group.
REFRAIN-PD study: REducing FRActures IN Parkinson’s Disease

Principal Investigator: Dr Emily Henderson, University of Bristol
Timescale: February 2023 – February 2025
Amount: £89,167
Summary: Older adults with neurological conditions are at higher risk of falling and breaking bones. Unsteady walking, impaired memory and thinking, muscle weakness and osteoporosis (fragile bones) all contribute to these risks of falls and breaks. Broken bones cause pain, can require a major operation in hospital, and leave people with difficulties in their day-to-day life and activities. We will study bones in people with Parkinson's who are already part of our research programme. People will have additional scans of their whole body, spine, hip, wrist and leg to tell us about their bone strength, and an assessment of their muscle function. We will detect broken bones in the spine (which often go undiagnosed) and will compare findings with measures of their memory, physical abilities and other risk factors that might make broken bones more likely. This will mean we can: i. Better identify who is at risk of breaking bones ii. Discover how much bone scans help us to understand this risk iii. Find out whether patients are prescribed and taking the correct treatment iv. Update UK guidance we have previously produced for bone health treatment in Parkinson’s and similar conditions, to accord with new osteoporosis guidance.

Become a member today
Discover more about becoming an ROS member and getting exclusive access to updates about our research projects.

Give to support research
We receive no funding from the government therefore our research projects are dependent on the generosity of our supporters.
 Search
Search
 Login
Login


